It has been well-established that influenza vaccination reduces influenza-associated illness. CDC estimates that tens of thousands of hospitalizations are averted because of vaccination each year and that vaccination prevents millions of influenza-related illnesses. This is despite that fact that fewer than half of those over the age of 6 months are vaccinated each year. Higher vaccination rates almost certainly would prevent a substantial number of additional cases and hospitalizations.
The estimated number of flu illnesses prevented by flu vaccination during the 2017–2018 season: 7 million, about the population of New York City.
In the United States, goals for improving influenza vaccination rates are outlined in Healthy People 2020 (see table below). Since 2010 CDC has recommended that all people 6 months of age and older receive annual influenza vaccination. Despite substantial gains in the number of people vaccinated each year, we have yet to come close to the goal of universal influenza vaccination.
Flu Vaccination Coverage Among Adults by Age Group and Season, United States, 2010–2018
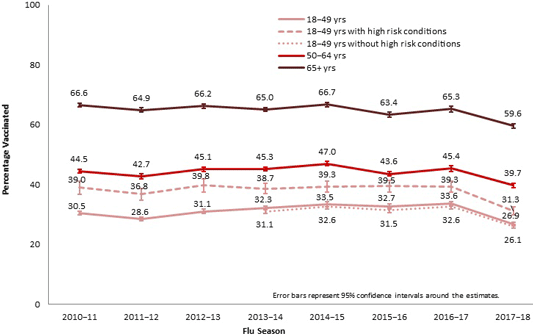
Source: CDC.
The College of Physicians of Philadelphia provides a fascinating look at the issues associated with vaccines on their History of Vaccines website (http://www.historyofvaccines.org/). It is well worth the time to look over this website and explore “the ways in which vaccines, toxoids, and passive immunization work, how they have been developed, and the role they have played in the improvement of human health.”
Vaccination Rates Among Adults
During the 2017–2018 season, flu vaccination coverage among adults was 37.1%, a decrease of 6.2% from the previous flu season. As in past years, people continued to get flu vaccinations through the winter and into spring. By the end of the 2017–2018 season, vaccine coverage for adults was approximately 8 percentage points higher than early-season estimates.
Early-season 2018–19 estimates show an increase in flu vaccination coverage among adults compared to the previous season. However, vaccination coverage varied by age group and state (CDC, 2018f).
Early and End of Season Flu Vaccination Coverage Among Adults, United States, 2014–November 2018
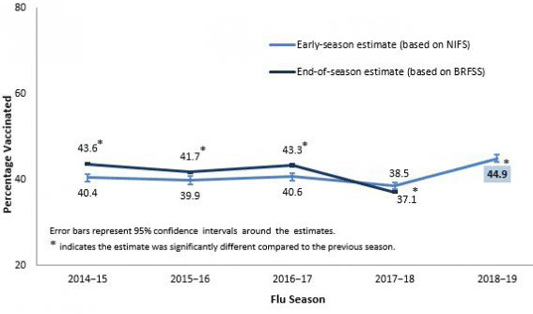
Source: CDC.
Flu vaccination coverage for the 2017–2018 season was lower for every age group compared to the previous year. For all adult age groups, flu vaccination rates were at their lowest levels compared with the seven previous seasons. There was large between-state variability in flu coverage among adults, ranging from 29.2% in Louisiana to 46.3% in West Virginia (CDC, 2018f).
Early findings show an increase in 2018-2019 flu vaccinations. Among children aged 6 months–17 years there was an increase of 6.8 percentage points to 45.6%, compared with the same time period the prior year. Flu vaccination coverage among adults aged ≥18 years increased by 6.4 percentage points to 44.9%. Coverage increased for children aged 6 months–12 years and among all adult age groups. Interpretation of these results should take into account limitations of the surveys, including reliance on self-report of vaccination status and decreasing response rates (CDC, 2018f).
Low vaccination rates have also been noted in Europe, where surveys from five countries have shown consistently low coverage in the general population. During the 2009 H1N1 pandemic, vaccination campaigns were adopted in many countries; however, low acceptance of a vaccine or uptake rates against pandemic influenza were reported in many studies (25% among health workers in Beijing, 17% among a French adult population, and 8.9% among pregnant women in Turkey) (Wu et al., 2013).
Vaccination Rates Decline as Clinic Day Progresses
A retrospective, quality-improvement study of 11 primary care practices at the University of Pennsylvania Health System from September 1, 2014, to March 31, 2017 yielded interesting results. Researchers found that influenza vaccination rates significantly declined as the clinic day progressed.
Offering an “active choice” intervention in which medical assistants were prompted to make decisions on whether to template vaccinations orders in patients’ electronic health record for clinicians to review was associated with a significant increase in vaccination rates. Importantly, the active choice intervention was associated with a significant increase in influenza vaccination rates that were similar in magnitude throughout the day.
Source: Kim et al., 2018.
Vaccination Rates Among Children
Influenza-associated deaths in children (less than 18 years) were added as a nationally notifiable condition in 2004. Of particular interest, for children in the United States, influenza vaccination rates are fairly high in young children but decrease with increasing age:
- 6–23 months: 76.3%
- 2–4 years: 66.2%
- 5–12 years: 59.9%
- 13–17 years: 48.8% (Black et al., 2017)
CDC analyzed data from the National Immunization Survey—Flu to estimate flu vaccination coverage for the U.S. population of children 6 months through 17 years during the 2018–2019 flu season. Receipt of flu vaccination was determined by parental report. Vaccination coverage varied by state and age group.
Estimates of flu vaccination coverage as of mid-November 2018 for children aged 6 months to 17 years was 45.6%, an increase of 6.8 percentage points compared with the same time period during the previous year (Xu et al., 2019).
During the 2018–2019 flu season, 116 laboratory-confirmed influenza-associated pediatric deaths (ages 2 months–17 years) were reported. Twenty-two percent of the deaths were associated with influenza A(H3N2) infection, 37% with influenza A(H1N1), 34% with an influenza A virus for which no subtyping was performed, 7% with an influenza B virus, and 1% with an influenza virus for which the type was not determined. The mean age of the pediatric deaths reported this season was 6.1 years and 66% of those children died after admission to the hospital. Among the 104 children with a known medical history, 51% had at least one underlying medical condition recognized by the Advisory Committee on Immunization Practices (ACIP) as placing them at high risk for influenza-related complications (Xu et al., 2019).
Among the 89 children who were eligible for influenza vaccination (age ≥6 months at date of onset) and for whom vaccination status was known, 34% had received at least 1 dose of influenza vaccine before illness onset (25 of the children were fully vaccinated according to 2018 ACIP recommendations, and five had received 1 of 2 recommended doses) (Xu et al., 2019).
Early and End of Season Flu Vaccination Coverage Among Children, United States, 2014–November 2018
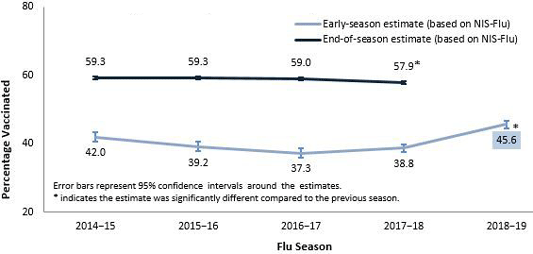
Source: CDC.
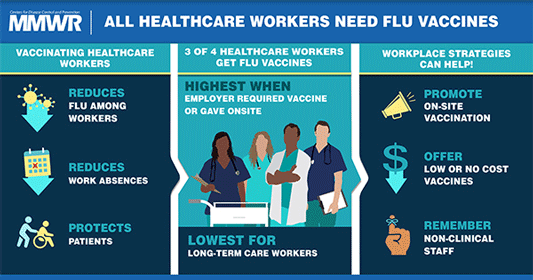
Vaccination Rates Among Healthcare Workers
The overall influenza vaccination coverage estimate among healthcare personnel was 78.4% during the 2017–2018 influenza season, a 15% increase since the 2010–2011 season, but similar to coverage during the previous four seasons. As in past seasons, the highest coverage was associated with workplace vaccination requirements. Reported coverage was consistently higher among healthcare personnel working in hospital settings than among those working in other settings; healthcare personnel working in hospital settings were also the most likely to report workplace vaccination requirements (Black et al., 2018).
Influenza vaccination coverage was higher among healthcare personnel with vaccination available at or promoted in their workplace than among those without any type of employer promotion of vaccination; however, coverage achieved through vaccine availability and promotion was still suboptimal in the absence of requirements. Neither vaccination coverage nor prevalence of employer vaccination requirements or promotion differed in the 2017–2018 season compared with the previous season, despite the severity of the 2017–2018 influenza season (Black et al., 2018).
Influenza vaccination coverage among healthcare personnel working in long-term care settings, the majority of whom work as assistants and aides, continues to be consistently lower than that among healthcare personnel working in all other healthcare settings. Influenza vaccination among healthcare personnel in long-term care settings is especially important because influenza vaccine efficacy is generally lowest among elders, who are at increased risk for severe disease (Black et al., 2018).
In contrast to healthcare personnel working in hospitals, a much lower proportion of survey respondents working in long-term care settings reported having a requirement for vaccination, and 23.5% reported that their employer did not require, make available on-site at no cost, or promote vaccination in any way. Implementing workplace vaccination programs that have been successful in increasing coverage in hospital settings, including vaccination requirements, could increase coverage in long-term care and other settings with historically lower vaccination coverage (Black et al., 2018).
Did You Know. . .
Workplace vaccination programs that have been successful in increasing coverage in hospital settings could be implemented in long-term care and other settings with lower vaccination coverage.
Employers can use the long-term care web-based toolkit developed by CDC and the National Vaccine Program Office to access resources, strategies, and educational materials for increasing influenza vaccination among healthcare personnel in long-term care settings (Black et al., 2017).
These low rates are certainly at least partly related to high staff turnover; it is not uncommon for a long-term facility’s staff to turn over completely every few years. Newly hired managers may not adhere to existing policies related to vaccinations, or they may decide to discard such policies and implement new ones (AHRQ, 2014).
Source: Morbidity and Mortality Weekly Report, 2018.
Vaccination Rates by Healthcare Occupation
[Material in this section from Black et a., 2017 unless otherwise cited.]
During the 2016–2017 season (earliest available statistics), flu vaccination coverage was highest among physicians (95.8%) and lowest among assistants and aides (69.1%), and highest overall among healthcare personnel who were required by their employer to be vaccinated (96.7%).
Among healthcare personnel working in settings where vaccination was neither required, promoted, nor offered onsite, vaccination coverage continued to be low (45.8%). An increased percentage of healthcare personnel reporting a vaccination requirement or onsite vaccination availability compared with earlier influenza seasons might have contributed to the overall increase in vaccination coverage during the past seven influenza seasons.
Vaccination Rates by Healthcare Setting
Not surprisingly, vaccination rates among healthcare providers vary by work setting. During the 2016–2017 season, vaccination coverage continued to be higher among healthcare personnel working in hospitals (92.3%) and lower among healthcare personnel working in ambulatory (76.1%) and long-term care settings (68%).
Coverage was highest among physicians, nurse practitioners/physician assistants, nurses, pharmacists, and healthcare personnel working in hospital settings. Coverage was lowest among assistants and aides and personnel working in long-term care settings. Employer vaccination requirements and offering vaccination at the workplace at no cost were associated with higher vaccination coverage.
Why is it so important to increase vaccination rates among healthcare personnel?
Because of their close proximity to sick patients, healthcare providers are more likely to get influenza and to pass it on, with more significant consequences than for any other group of workers. Paradoxically, when a healthcare provider gets sick, several studies have shown that more than 75% continue to work despite being infected with influenza (Riphagen-Dalhuisen et al., 2013).
A recent study conducted among nursing home workers in France suggest low rates of influenza vaccination there as well. Management and working environment appear to play a strong role and the authors suggest that: “To overcome vaccine ‘hesitancy,’ specific communication tools may be required to be adapted to the various NH professionals to improve influenza prevention” (Elias et al., 2017).
