Behavioral and psychological symptoms of dementia (BPSD) or neuropsychiatric symptoms of dementia (NSP) occur in up to 90% of patients with dementia (Passmore, 2013). Neuropsychiatric symptoms can range from mild (depression, anxiety, irritability, apathy) to severe (agitation, aggression, vocalizations, hallucinations, disinhibition,* among others). Symptoms can persist or recur over time and are associated with patient and caregiver distress, increased rates of institutionalization, and increased mortality (Nowrangi et al., 2015).
*Disinhibition: a loss of inhibition, a lack of restraint, disregard for social convention, impulsiveness, poor safety awareness, an inability to stop strong responses, desires, or emotions.
Management of neuropsychiatric symptoms of dementia relies on the use of both pharmacologic and non-pharmacologic therapies based on treatments developed for other psychiatric disorders. Unfortunately, there has been a lack of progress in the development of effective treatments due to an incomplete understanding of the biological mechanisms underlying these symptoms. Because of this, treatment strategies are in response to behaviors and largely based on observation and experience rather than on an understanding of the underlying cause (Nowrangi et al., 2015).
Among the many neuropsychiatric behaviors associated with Alzheimer’s disease and other types of dementia, depression,* apathy, agitation and aggression, and delusions and hallucinations (psychoses) are some of the most common. Challenging behaviors such as wandering, rummaging and hoarding, and sleep disturbances can arise and may or may not be related to neuropsychiatric changes.
*See Module 4: The 3 D’s: Dementia, Delirium, and Depression for more on depression.
Non-Pharmacologic Approaches
There is growing evidence to suggest that the management of neuropsychiatric behaviors (particularly in long-term care) should shift from the traditional practice of medication-based symptom management to comprehensive non-pharmacologic approaches aimed at maintaining the physical and emotional comfort of the individual. Such non-pharmacologic interventions can be used with the individual or can be applied to the physical setting or built environment (Soril et al., 2014).
Non-pharmacologic treatments for the challenging behaviors associated with dementia include cognitive stimulation, cognitive training, behavioral interventions, exercise, music, aromatherapy, bright light therapy, animal therapy, and multi-sensory stimulation (Snoezelen*), among others. Non-pharmacologic interventions can also be aimed at caregivers and include education, support, case management, and respite care (Nowrangi et al., 2015).
*Snoezelen: a Snoezelen or controlled multisensory environment room uses light, sound, scents, and music to initiate sensations. These have both relaxing and activating effects on the various parts of the brain related to sensory perception. The specific design directs and arranges the stimuli; it creates interest, brings back memories and guides relationships.
Behavior therapy using antecedent-behavior-consequence (ABC), also called a problem-solving approach, may provide sustained improvements in behavior. One meta-analysis found that behavioral management techniques focused on individual patients’ behavior and individually oriented techniques provided longer-lasting (several months) positive effects on behavior when compared with placebo (Nowrangi et al., 2015).
Other studies have shown that staff education leads to reductions in behavioral outbursts and fewer episodes of restraint use. In a meta-analysis by Olazarán and colleagues, the majority of the studies reviewed showed positive effects for improvements in mood, behavior, and quality of life of persons with dementia while delaying institutionalization (Nowrangi et al., 2015).
One effective non-drug approach used to address challenging behaviors associated with dementia encourages caregivers to problem solve—to look for and understand the root cause of a behavior. Treatment can include solving problems within the environment, managing medication issues, and brainstorming with caregivers. The problem-solving approach encourages caregivers and healthcare workers to identify critical points for intervention based on observing the antecedent, behavior, and consequence (A, B, C) of a challenging behavior.
- Antecedent—what caused the behavior?
- Behavior—what is the behavior?
- Consequence—what are the consequences of the behavior?
The ABC problem-solving approach is particularly effective when successful strategies are shared by staff, caregivers, and family members and used to uncover the cause of a particular behavior. The ABC method helps staff and caregivers understand when and how often a behavior occurs and offers the opportunity for discussion and planning.
In Norway, researchers worked with healthcare workers in a small rural nursing home to identify the effectiveness of the problem-solving approach in addressing challenging behaviors in residents with dementia. At the start of the study the healthcare workers described what they understood about—and how they responded to—challenging behaviors. Most regarded challenging behaviors as a symptom of dementia, including physical attacks, such as hitting, spitting, and pinching (Lykkeslet et al., 2014).
One of the care workers described her reaction to the behavior of a female patient:
I do not think she always knows that she pinches us. . . then we try to get away. . . we pretend that nothing has happened and her behavior is a great challenge to us, because her inhibitions against hitting and kicking are very low.
Residents who wandered around or repeatedly said that they wanted to go home were also identified as a challenge. The caregivers regarded such behavior as a symptom of dementia that affected other residents. They noted that when one patient wants to go home, others also want to go home Lykkeslet et al., 2014).
All the time she wants to go someplace, but does not know where. She puts on a lot of clothes and walks around. . . if I tell her the truth about where she is she becomes irritated, resigned, or offended.
During the course of the first year of the study the staff reported that, as a result of being encouraged to look for the cause of a behavior, they began to get into the habit of searching for meaning in patients’ behavior and gradually began to change their attitude toward the people they were caring for. Health workers claimed they were learning to see peculiar behavior more as a result of a challenging situation than as a symptom of a difficult patient (Lykkeslet et al., 2014).
One of the workers gave an example of a patient who did not want to eat her food:
She refuses to open her mouth, so it is impossible to feed her. Any new caregiver who helps her will often fail. When I assist her, I always start by touching her hand, holding her hand, and then she gradually starts to eat.
The care worker added that this patient might have misunderstood the situation and therefore did not trust the new caregiver, who had to spend some time building trust.
You cannot go straight to the task—she needs some preparation to understand what is going on and what she has to do.
By observing the patient’s reactions, the care worker understood that the patient needed time to prepare. She needed to understand that the situation was a meal and that the care worker wished her well (Lykkeslet et al., 2014).
Another care worker told about how she began to understand patients with poor verbal language.
We try to read their body language. Perhaps she is in pain. . . sometimes she can tell us. . . other times we get no answer.
Sometimes the care workers saw the behavior as a response to a critical situation (“because he is vulnerable he becomes angry”). As the study progressed, researchers began to observe changes in the care provider’s attitudes and approach to activities. They noted that when the caregivers experienced a situation as challenging, they more frequently started to reflect on the patients’ needs (Lykkeslet et al., 2014).
For pragmatic suggestions that healthcare workers can use when working with individuals who can no longer express themselves appropriately, see ATrain’s course entitled Dementia Care: Common Sense Guidelines.
Dementia and Apathy
Apathy is described as a lack of interest or emotion and may be an early symptom of cognitive impairment, especially in frontal-temporal dementia. The prevalence of apathy increases with the severity of dementia. Apathy is different from depression although apathy and depressive symptoms may occur together (Volicer & van der Steen, 2014).
For a diagnosis of apathy, the diminished motivation must persist for no less than four weeks, and two of the following three dimensions should be present:
- Reduced goal-directed behavior
- Reduced goal-directed cognitive activity
- Reduced emotions (Rea et al., 2014)
Although apathy is a common behavioral symptom of neurodegenerative and other brain disorders it is one of the most under-recognized, under-diagnosed, and poorly managed aspects of these diseases (Leroi & Robert, 2012). It is the cause of distress for caregivers because it places the responsibility for day-in and day-out decisions on the caregiver. Over time, anger and conflicts inevitably follow between patients and caregivers. This makes apathy a risk factor for institutionalization (Rea et al., 2014).
Causes of Apathy
Location of the Amygdala in the Human Brain
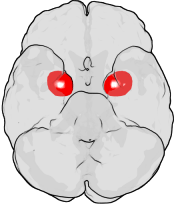
The figure shows the underside of a human brain, with the front of the brain at the top. The red areas show the approximate location of the amygdala in the temporal lobes of the human brain. Source: Wikimedia Commons.
In Alzheimer’s disease, apathy is associated with loss of nerve cells within specific parts of the brain. In the past, apathy was classified as a motivational loss not attributable to emotional stress, cognitive impairment, or consciousness reduction. Apathy has since been related to disconnection of certain brain circuits, including the amygdala,1 which receives nerve impulses from various parts of the brain. This suggests that impaired cholinergic neurotransmission2 is involved in apathy pathophysiology (Rea et al., 2014).
1Amygdala: part of the limbic system, associated with memory, decision-making, and emotions.
2Cholinergic neurotransmission: a receptor is cholinergic if it uses acetylcholine as its neurotransmitter. The cholinergic system is involved in the regulation of memory and learning.
Management of Apathy
At present apathy accompanying Alzheimer’s disease is a disorder not largely investigated and its treatment remains a challenge. Only a few treatments have been proposed, but so far there is no clear demonstration of the advantage of one treatment over others (Rea et al., 2014).
Four categories of drugs are currently used to treat apathy in people with Alzheimer’s dementia. These include:
- Cholinesterase inhibitors (inhibits the breakdown of acetycholine)
- Monoaminergic agents such as methylphenidate (Concerta, Methylin, Medikinet, Ritalin) and modafinil (Provigil)
- Drugs such as the Ginkgo biloba extract Egb 76
- Selective serotonin reuptake inhibitor citalopram (Celexa) (Rea et al., 2014)
Agitation and Aggression
The terms agitation and aggression are often used in reference to behavioral symptoms associated with dementia. Agitation refers to observable, non-specific, restless behaviors that are excessive, inappropriate, and repetitive. This can include verbal, vocal, or motor activity (Burns et al., 2012).
Aggression involves physically or verbally threatening behaviors directed at people, objects, or self. Aggressive behaviors are generally perceived as a threat to the safety of those with dementia and to those around them, which includes family caregivers, staff, and other residents. Aggression is often described by specific acts such as:
- Verbal insults
- Shouting, screaming
- Obscene language
- Hitting, punching, kicking
- Pushing and throwing objects
- Sexual aggression (Burns et al., 2012)
Agitation and aggression occur in about 50% to 80% of nursing home residents with cognitive impairments (Ahn & Horgas, 2013). Men are more likely than women to engage in aggressive behaviors. Cognitively impaired people are more likely to engage in non-aggressive physical behaviors (such as pacing). Functionally impaired people are more likely to engage in verbally agitated behaviors (complaining, vocal outbursts) (Pelletier & Landreville, 2007).
Causes of Agitation and Aggression
Agitated and aggressive behaviors are a type of communication often related to feelings of helplessness, loss of control, discomfort, pain, or fear. Agitation and aggression can be a response to a violation of personal space or a perceived threat. These behaviors often occur during personal care tasks involving close caregiver-resident contact (Burns et al., 2012).
Physiologically, aggression may be related to a decrease in the activity of serotonin or reduced transmission of acetylcholine in the brain. Frontal lobe dysfunction has also been implicated. Aggression may also be related to underlying depression or psychotic symptoms (Burns et al., 2012).
Pain severity is associated with the frequency of agitated and aggressive behaviors. Nursing home residents with more severe pain are more likely to display these behaviors (Ahn & Horgas, 2013).
Management of Agitation and Aggression
To understand and prevent agitation and aggression, consider the antecedent: What precipitated the behavior? Observe the person and try to determine the cause of the agitation. Look for patterns. Use one of the many available rating scales—such as the Rating Scale for Aggressive behavior in the Elderly (RAGE)—to assess aggressive behaviors. For agitated behaviors rating instruments such as the Brief Agitation Rating Scale can be used to assess the different aspects of agitation (Burns et al., 2012).
Psychosocial and environmental interventions can reduce or even eliminate agitated or aggressive behaviors. Music therapy, massage, craniosacral therapy,* therapeutic touch, acupressure, and tactile massage have been shown to be successful for treating aggression. In addition, individual behavioral therapy, bright light therapy, Montessori activities, and individualized person-centered care based on psychosocial management is recommended (Burns et al., 2012).
*Craniosacral therapy: a hands-on technique that uses soft touch to release restrictions in the soft tissue surrounding the central nervous system.
For people with dementia, antipsychotics may reduce aggression and psychosis, particularly among those most severely agitated. However, in older people, antipsychotics are associated with increased overall mortality, worsening cognitive impairment, hip fracture, diabetes, and stroke (Jordan et al., 2014).
My mom Kimberly has dementia and my sister and I take turns staying with her at her home. She’s a pretty quiet person but a couple of years ago she starting getting really agitated and angry in the evening—we blamed this on her dementia. It got so bad that we thought about sedating her but a nurse practitioner suggested we try to figure out what was causing her agitation using the problem-solving approach.
We watched her behavior carefully and finally figured out that she was getting really cold in the evening—even when it was warm outside. She didn’t tell us she was cold but when we asked she said “I’m freezing.”
Once we realized what was wrong, we ordered special heated slippers and also got an electric mattress pad so her bed is nice and warm when she goes to bed. It sounds simple but it took us a long time to figure it out because she doesn’t complain. Now she’s rarely—actually she’s never—agitated or angry in the evening!
Family Caregiver, Santa Rosa, California
Delusions and Hallucinations (Psychosis)
Psychosis is a disturbance in the perception or appreciation of objective reality (Burns et al., 2012) and can include delusions and hallucinations. A delusion is a false idea or belief or a misinterpretation of a situation. Hallucinations are sensory events in which a person hears, tastes, smells, sees, or feels something that is not there.
Delusions and hallucinations can occur in people with dementia, with hallucinations particularly common in those with Parkinson’s disease dementia and Lewy body dementia. In fact, the presence of recurrent visual hallucinations has been identified as one of the core features in the clinical diagnosis of dementia with Lewy bodies. Delusions and hallucinations can trigger other neuropsychiatric symptoms, such as agitation or aggression, which can lead to early nursing home admission (Vermeiren et al., 2015).
Causes of Psychosis
Delusions and hallucinations can be caused by health factors such as urinary tract infections, environmental factors such as poor lighting or sensory overload, or a reaction to certain medications. Changes in the brain can also contribute to these behaviors, especially changes related to sensory awareness, memory, and decreased ability to communicate or be understood.
People suffering from delusions and paranoia can become suspicious of caregivers or friends. Sensory deficits can contribute to delusions and hallucinations due to the distortion of sound or sight.
Visual hallucinations can occur in the moderate to severe stages of dementia and are particularly common in those with Lewy body dementia. While atypical antipsychotics are sometimes used off-label to manage hallucinations, in a person with Lewy body dementia antipsychotic medications can make hallucinations worse. In a person with new onset of visual hallucinations, the number one cause is medication side effects. For this reason, all medications should be carefully reviewed. This includes prescription and over-the-counter (OTC) medications, as well as herbal supplements.
Management of Psychosis
The first step in the management of delusions and hallucinations is to rule out delirium as a cause (see Module 4 for more on delirium). Another important factor is to determine if the claims by the person with dementia actually did occur (Burns et al., 2012).
At present, antipsychotics are the primary pharmacologic treatment option used to alleviate depression and psychosis in Alzheimer’s disease—although they may induce serious side effects, increase mortality rates, and their efficacy is “modest” at best. The administration of psychotropic medication has also been associated with a more rapid cognitive and functional decline, and not necessarily with improved neuropsychiatric symptoms (Vermeiren et al., 2015).
The pharmacologic treatment of neuropsychiatric symptoms of dementia in those with dementia with Lewy bodies requires a cautious approach. All drugs with anticholinergic side effects, such as tricyclic antidepressants, low potency neuroleptics, antiparkinsonian anticholinergic drugs, and antispasmodics for bladder or gastrointestinal tract, should be avoided due to their potential to exacerbate psychotic symptoms. Finally, the administration of memantine (Namenda) may result in variable symptomatic side effects in patients with dementia with Lewy bodies, including worsening of psychosis or even an adverse drug reaction (Vermeiren et al., 2015).
From a non-pharmacologic standpoint, psychotic behaviors can often be successfully managed by observing the behavior and listening to what the person experiencing the paranoia or delusion has to say. Is the feeling pleasant or frightening? If the hallucination elicits a fearful or negative response, address the person’s need to regain comfort. For example, you may ask “What will make you feel safe or comfortable?”
When communicating with someone who is expressing paranoia or delusions, realize that even if their complaint is not true, it is real for that person. It is best not to argue; simply explaining the truth of the situation will not work. Do not agree with the person or further validate the paranoia or delusion, but respond to the person’s emotion.
Decreasing auditory and visual stimuli can help in managing hallucinations. It may also be helpful to have the person evaluated for visual or hearing impairment. Delusions and hallucinations can be addressed using behavioral interventions or, in some cases, antipsychotic medication (Burns et al., 2012).
Here are some other suggestions for addressing hallucinations:
- Reduce stimulation in the environment—minimize violent or noisy TV, remove wall hangings, reduce noise, play relaxing music.
- Cover mirrors.
- Reduce glare from windows.
- Ensure adequate lighting.
- Review medications for potential side effects.
