
Source: CDC.
The COVID-19 pandemic continues to devastate the United States and the world, with the death toll approaching 1,000,000 Americans; however, not all communities have been affected equally. It is clear that some racial and ethnic minority groups are being affected by COVID-19 in much greater numbers than non-Hispanic White and Asian Americans.
Conditions in the places where people live, learn, work, play, and worship affect a wide range of health risks and outcomes, such as COVID-19 infection, severe illness, and death. These conditions are known as social determinants of health. Long-standing inequities in social determinants of health that affect these groups, such as poverty and healthcare access, are interrelated and influence a wide range of health and quality-of-life risks and outcomes. Because of these inequities, people from some racial and ethnic minority groups are less likely to be vaccinated against COVID-19 than non-Hispanic White people (CDC, 2020, December 10).
Populations with Social Inequities
African Americans, Native Americans, and Hispanic people are dying at rates much greater than their population share. Among cases with known race and ethnicity, 33% were Hispanic, 22% were Black, and 1.3% were American Indian or Alaska Native. For example, during the first 3 months of the COVID pandemic, Native Americans accounted for 58% of COVID-related deaths in New Mexico despite making up just 11% of the population (Sequist, 2022). Recent studies have shown that minority children are also being disproportionately affected.
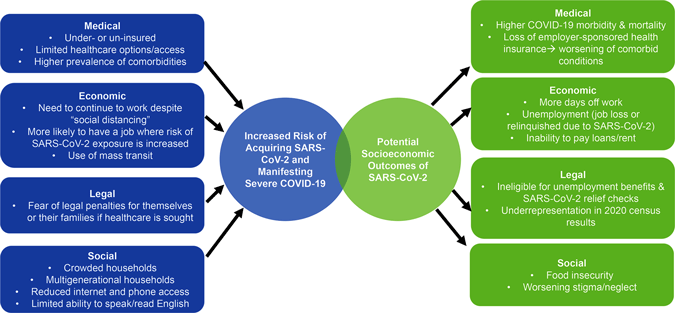
Other vulnerable populations, particularly immigrant communities that have similar socioeconomic status and rates of comorbidities, are also being hit hard by the coronavirus. There are over 46.7 million immigrants currently living in the United States, of which 11 million are undocumented. Poverty, limited access to healthcare, and fear of legal repercussions place vulnerable immigrant communities within the United States at high risk for acquiring SARS-CoV-2 and developing severe COVID-19 illness (Clark et al., 2020).

Source: NIH.
Longstanding systemic health and social inequities have put many people from racial and ethnic minority groups at increased risk of getting sick and dying from COVID-19. The term racial and ethnic minority groups includes people of color with a wide variety of backgrounds and experiences. But some experiences are common to many people within these groups and social determinants of health, such as poverty and healthcare access, have historically prevented them from having fair opportunities for economic, physical, and emotional health (CDC, 2020a).
As in past pandemics, social and economic determinants strongly influence susceptibility to and health outcomes of COVID-19. Health differences between racial and ethnic groups result from inequities in living, working, health, and social conditions that have persisted across generations (CDC, 2020a).
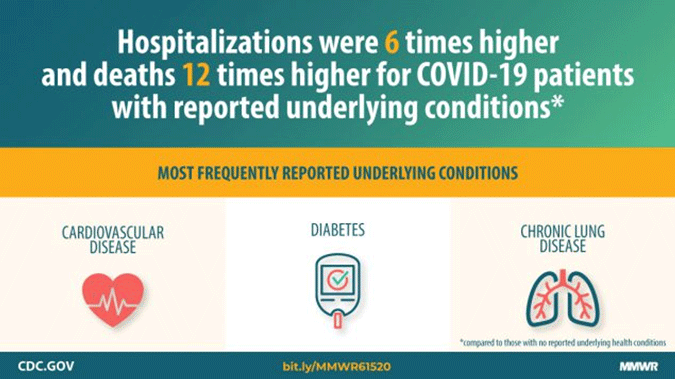
Illnesses such as heart disease, diabetes, and lung disease are more prevalent in African American, American Indian, and Hispanic communities. Unfortunately, these diseases are also leading risk factors for severe disease and death from COVID-19 (Nania, 2020).
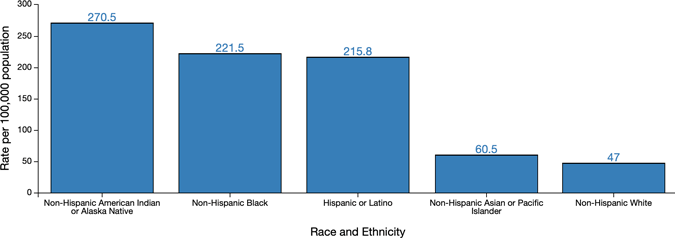
Hospitalization Rates
Among some racial and ethnic minority groups—including African Americans, Hispanics, American Indians, and Alaska Natives—evidence points to higher rates of hospitalization from COVID-19 than among non-Hispanic white persons. As of July 4, CDC data shows (CDC, 2020b):
- American Indians or Alaska Natives have an age adjusted hospitalization rate approximately 5.7 times that of non-Hispanic white persons
- Black people have a hospitalization rate approximately 4.7 times that of non-Hispanic white persons
- Hispanic or Latino persons have a hospitalization rate approximately 4.6 times that of non-Hispanic white persons
Age-adjusted COVID-19-associated Hospitalization Rates by Race and Ethnicity, COVID-NET, March–July 4, 2020
Death Rates
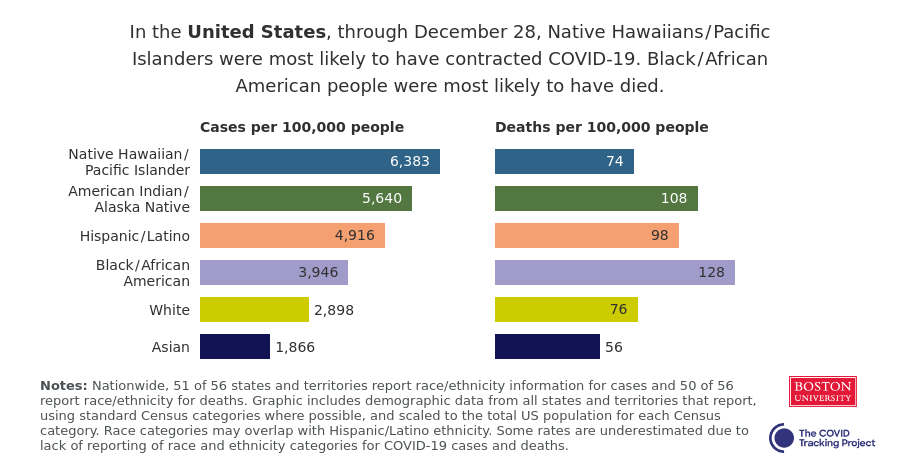
According to the CDC, in 35 of the 47 states that report racial statistics of the pandemic, Black people generally had disproportionately high death rates—more than twice as high as white and Asian Americans. American Indians and Alaska Natives were highest in five states, Asian Americans in four states, white Americans in two states, and Native Hawaiian and Pacific Islanders in one state (Baranauckas et al., 2020).
As of December 28, 2020, statistics show death rates for all Americans are as follows (COVID Tracking Project, 2020):
- Black Americans: 128 deaths per 100,000
- American Indians: 108 deaths per 100,000
- Pacific Islander Americans: 74 deaths per 100,000
- Hispanic Americans: 98 deaths per 100,000
- White Americans: 76 deaths per 100,000
- Asian Americans: 56 deaths per 100,000
Factors That Increase Risks From COVID-19
Living Conditions
For many people from racial and ethnic minority groups, living conditions can contribute to poor health conditions and make it harder to follow steps to prevent getting sick with COVID-19 or to seek care if they do get sick.
Members of racial and ethnic minorities are more likely to live in densely populated areas because of institutional racism in the form of residential housing segregation. In addition, overcrowding is more likely in tribal reservation homes and Alaska Native villages compared to the rest of the nation. People living in densely populated areas and homes may find it harder to practice social distancing (CDC, 2020a).
Racial housing segregation is linked to health conditions (e.g., asthma and other underlying medical conditions) that put people at increased risk of getting severely ill or dying from COVID-19. Some communities with higher numbers of racial and ethnic minorities also have higher levels of exposure to pollution and other environmental hazards (CDC, 2020a).
Homes on Native American reservations are more likely to lack full plumbing when compared to the rest of the nation, making handwashing and disinfection harder.
Many members of racial and ethnic minority groups live in neighborhoods that are far from grocery stores and medical facilities, and may lack safe and reliable transportation, making it harder to stock up on supplies that would allow them to stay home and to receive care if sick.
Members of racial and ethnic minority groups may be more likely to rely on public transportation, which makes it challenging to practice social distancing.
People living in multigenerational households and multifamily households (more common among some racial and ethnic minority groups), may find it hard to protect older family members or isolate those who are sick if space in the household is limited.
Work Circumstances
Some types of work and workplace policies can put workers at increased risk of getting COVID-19. Members of racial and ethnic minority groups are more likely to work in these conditions (CDC, 2020a).
The risk of infection is greater for workers in essential industries such as healthcare, meat-packing, groceries, and factories. These workers cannot work from home and must be at the job site despite outbreaks in their communities, and some may need to continue working due to economic circumstances. Many essential workers in lower paying jobs do not get paid sick leave and thus may be more likely to keep working when they are sick (CDC, 2020a).
On average, racial and ethnic minorities earn less than non-Hispanic whites, and have less accumulated wealth, lower levels of education, and higher rates of joblessness. These factors affect the quality of the social and physical conditions in which people live, learn, work, and play, and can have an impact on health outcomes (CDC, 2020a).
Healthcare Inequities and Underlying Conditions
Compared to non-Hispanic whites, Hispanics are almost 3 times as likely to be uninsured, while African Americans are almost twice as likely to be uninsured. In all age groups, Blacks are more likely than non-Hispanic whites to report not being able to see a doctor in the past year because of cost. In 2017 almost 3 times as many American Indians and Alaska Natives had no health insurance coverage compared to non-Hispanic whites (CDC, 2020a).

Source: National Institutes of Health.
Racism and systemic inequities undermine prevention efforts, increase levels of chronic and toxic stress, and ultimately sustain health and healthcare inequities. Minorities may not receive care because of distrust of the healthcare system, language barriers, or cost of missing work (CDC, 2020a).
Underlying medical conditions put people at increased risk for severe illness from COVID-19. Compared to non-Hispanic whites, Blacks experience higher rates of chronic conditions at earlier ages as well as higher death rates. American Indian and Alaska Native adults are more likely to be obese, have high blood pressure, and smoke cigarettes than non-Hispanic white adults (CDC, 2020a).
Poor healthcare and poor nutrition contribute to conditions like high blood pressure, diabetes, heart disease, and lung disease that are the most commonly reported illnesses in people with severe outcomes from COVID-19 (CDC, 2020a).
Source: CDC.gov.
African Americans
“We have a particularly difficult problem of an exacerbation of a health disparity,” Anthony Fauci, M.D., director of the National Institute of Allergy and Infectious Diseases, said at a recent White House coronavirus task force briefing. The things that get people into intensive care and require them to be put on a ventilator — something that often leads to death — are the very factors, Fauci said, “that are, unfortunately, disproportionately prevalent in the African American population” (Nania, 2020).
Infection and Death Rates Among African Americans
In the United States, Black people are dying at 2.8 times the rate of white people. More than 52,000 Black lives have been lost to COVID-19 since the pandemic began. Black people account for 17% of COVID-19 deaths where race is known (Atlantic, 2020).
There are eight states in the United States where the African American death rate is twice the share of the population. The largest disparities are seen in the states of Kansas and Wisconsin. In these two states, Black people make up only 6% of the population, but 29% and 26% of deaths from COVID-19, respectively. Black people make up 12% of the population of Missouri, but account for 37% of coronavirus deaths (Pew Research Center, 2020).
In New York State, Black people account for 33% of COVID-19 hospitalizations but make up only 18% of the state’s population. They are dying of coronavirus twice as often as white people in New York City, according to early data (WebMD, 2020).
Health Disparities in African American Communities
Increased coronavirus cases and deaths among African Americans can be linked to the same factors that are affecting other minority communities. Discrimination exists in systems meant to protect well-being or health, including healthcare, housing, education, criminal justice, and finance. Discrimination, which includes racism, can lead to chronic and toxic stress, and shapes social and economic factors that put some people from racial and ethnic minority groups at increased risk for COVID-19 (CDC, 2020a).
African Americans are more likely than white people to live in densely populated, unsafe areas with less green space, fewer healthy food options, and less access to healthcare. Social distancing is difficult in crowded neighborhoods and unhealthy food and inadequate healthcare leads to chronic health conditions that make people in these neighborhoods more likely to have serious outcomes from the coronavirus (Brookings, 2020).
Black people are less likely to have health insurance and less likely to seek healthcare because they tend to distrust the government and the medical establishment that are responsible for inequities in their treatment. Incidents like the Tuskegee Study of Untreated Syphilis in the African American Male and sterilization without people’s permission have made many Black people distrustful of the medical system (CDC, 2020a).
About a quarter of all public transit users are African Americans and they are more likely than whites to be so-called essential workers and unable to work from home, further heightening their exposure to other people. “Blacks represent nearly 30% of bus drivers and nearly 20% of all food service workers, janitors, cashiers, and stockers. During a highly contagious pandemic like COVID-19, Black workers, and consequently their families, are overexposed” (Brookings, 2020).
The highly contagious coronavirus spreads easily and rapidly in high-density communities that are filled with people who may have underlying health problems and cannot social distance or work from home. Chronic underlying health conditions make people more likely to have severe outcomes from this disease.
American Indians and Alaska Natives
If Native American tribes were counted as states, the five most infected states in the country would all be native tribes, with New York dropping to No. 6, according to a compilation by the American Indian Studies Center at U.C.L.A.
Kristof, 2020, May 30
Data collected as of December 28, 2020 indicate that American Indians and Alaska Natives have a death rate of 108 deaths per 100,000 people compared to 76 deaths per 100,000 in non-Hispanic white communities and 56 deaths per 100,000 in Asian American communities (APM Research, 2020).
This crisis—and the underlying conditions tribal communities face—are the result of centuries of colonial violence and neglect that continue to this day.
Doshi et al., 2020
Even before the pandemic, American Indians and Alaska Natives had shorter life expectancies than most other Americans. Lower life expectancy and a disproportionate disease burden exist because of inadequate education, disproportionate poverty, discrimination in the delivery of health services, and cultural differences. These are broad quality-of-life issues rooted in economic adversity and poor social conditions (IHS, 2019).

Source: Center for American Indian Health.
The U.S. government signed treaties with tribal nations when their lands and resources were taken from them, ensuring the “promise of all proper care and protection.” This trust responsibility included a “legal obligation to defend tribal treaty rights, lands, assets, and resources, as well as a duty to provide health services.” Unfortunately, there is a tradition of underfunding the Indian Health Service which is therefore unable to provide adequate health care for Native Americans (Warne & Frizzell, 2014). Only $3,943 is provided by the U.S. government to the Indian Health Service for Native American healthcare while the Bureau of Prisons spends $8,603 for each prisoner’s healthcare (Kristof, 2020, May 30).
American Indians and Alaska Natives born today have a life expectancy that is 5.5 years less than other Americans when all races are combined (73.0 years to 78.5 years, respectively). Heart disease, cancer, unintentional injuries, and diabetes are leading causes of death in American Indians and Alaska Natives. Chronic liver disease and cirrhosis, assault/homicide, intentional self-harm/suicide, and chronic lower respiratory disease all occur at much higher rates in indigenous people than in other Americans. Because of these underlying conditions, COVID-19 is hitting Native Americans and Alaska Natives particularly hard (IHS, 2019).
The Navajo Nation
The Navajo nation is the largest reservation in area in the United States, spread out over parts of Arizona, New Mexico, and Utah. It is suspected that the virus arrived there in early March 2020 when someone infected with the virus attended a Christian revival on the reservation. The virus then spread widely through community events and as a result of crowded living conditions. Social distancing is not possible in the small and crowded Native homes and, since 40% of reservation homes lack running water, hand washing is difficult. Coronavirus testing came back 28% positive compared to 8.7% nationally during the first week of July 2020 (Kristof, 2020 May 30; CDC, 2020a).

The Azhe’é Bidziil (Strong Fathers) program is based on evidence-based programs designed in collaboration with the Navajo Nation, White Mountain Apache Tribe, and the Johns Hopkins Center for American Indian Health. Source: Center for American Indian Health.
It has been difficult to gain a true understanding of the impact of COVID-19 on American Indian/Alaska Native communities. They are often designated as “other” when racial data is collected or categorized as Hispanics due to surnames or appearance, which could cause an undercount of the pandemic’s severity. A real picture of how the virus is affecting these communities would enable targeted solutions to help stop the spread, such as supplies of water, improved plumbing facilities, increased access to healthcare, and health literature translated into languages other than English (PBS Newshour, 2020).
Hispanics
Hispanics make up an increasing proportion of deaths in the United States from COVID-19. By the beginning of December 2020, more than 25,000 had lost their lives to the disease, accounting for nearly 14% of all deaths among Hispanic people (Thebault & Fowers, 2020).
Although Hispanics in the United States have a long life-expectancy (81.8 years), they endure poverty, discrimination, and lower rates of health insurance than both whites and Blacks. A study published June 18, 2020 in the Journal of the American Medical Association found that Hispanics are disproportionately affected by the coronavirus. Out of a total of 38,000 people tested for COVID-19 at Johns Hopkins Health System in the Washington DC area, 16% overall were positive. But, of 4,169 Hispanic people tested during the study, almost 43% were positive (US News and World Report, 2020).
Recent data made available by the CDC show that this disease disparity holds true throughout the United States and in all age groups. Data from New Jersey show that although 19% of the total population in that state is Hispanic they make up 30% of COVID-19 cases. In Utah, 14% of the total population is Hispanic but they account for 38% of COVID-19 cases. In Washington State, 13% of the total population is Hispanic, but they make up 34% of the COVID-19 cases (Calo et al., 2020). In California, Hispanic residents make up about 55% of the more than 356,000 infections while they make up just 39% of the state’s population (Yoon-Hendricks, 2020, July 16).
Partial COVID-19 death data show that Hispanic people are also dying at a rate above what population data would suggest. For example, CDC population data show that in Pennsylvania, where Hispanic people make up 7.6% of the total state population, 11% of COVID-19 deaths were among Hispanic people. In the United States as a whole, over 26% of COVID-19 deaths were among Hispanic people, who represent only 18% of the total U.S. population. (Calo et al., 2020).
The Vulnerability of Hispanic Communities
Vulnerability to COVID-19 can arise from many factors, including differential exposure, susceptibility, language barriers, and lack of access to health care.
Work Circumstances
Many Hispanic people work in frontline jobs in grocery stores, waste management, cleaning and sanitation services, and food delivery, putting them at constant exposure to people or materials that may be infected with COVID-19 (Calo et al., 2020).
Living Conditions
In addition to work circumstances, living conditions may also increase exposure to COVID-19 among Hispanic families. Twenty-five percent of Hispanic people live in multigenerational households (compared with only 15% of non-Hispanic white people), which makes it challenging to protect older family members or to isolate those who are sick if space in the household is limited (Calo et al., 2020).
Chronic Illness
Although having a chronic disease does not increase the risk of contracting the new coronavirus, the presence of chronic disease can worsen the outcome of COVID-19. Emerging data from the State of New York show that among those who died of COVID-19 (23,083 people as of May 20, 2020), the leading underlying illnesses were hypertension (54% of deaths) and diabetes (36% of deaths). This is alarming for Hispanic people because they have higher rates of both hypertension and diabetes as compared with non-Hispanic white people (Calo et al., 2020).
Language Barriers and Access to Healthcare
The lack of reliable information in Spanish has impeded efforts to combat the spread of the virus in Hispanic communities among those with language barriers, making them more likely to be unaware of best practices. In addition, Hispanic people are the largest population segment without healthcare insurance in the United States, leaving those with presumptive symptoms or with a positive COVID-19 test having limited access to needed healthcare (Calo et al., 2020).
Immigrants and COVID-19
[Material in this section is from Clark et al., 2020 unless otherwise cited.]
Poverty, limited access to healthcare, and fear of legal repercussions place vulnerable immigrant communities within the United States at high risk for acquiring SARS-CoV-2 and developing severe COVID-19. There are over 46.7 million immigrants currently living in the United States, of which 11 million are undocumented.
Houston is an example of a large, prosperous U.S. city that has a significant population of immigrants (and is dependent upon them). Currently, there are an estimated 1.6 million immigrants (23.3% of the population) living in Houston; they emigrated from Mexico (40.2%), El Salvador (7.6%), Vietnam (5.9%), India (5.5%), and Honduras (3.6%). More than 500,000 of these immigrants (37.2%) are undocumented. In Texas as a whole, an estimated 32% of undocumented immigrants live below the poverty level and 64% are uninsured, with limited options to meet their medical needs.
Disproportionate Impact of the COVID-19 Pandemic on Immigrant Communities in the United States
Source: PLOS.org.
As with other minority groups, the lack of readily accessible, affordable healthcare is particularly consequential during the COVID-19 pandemic. Early diagnosis and monitoring of persons with COVID-19 is critical both to optimize the individual patient’s outcome and to prevent further community transmission. Many vulnerable immigrants are under- or un-insured and thus depend upon Federally Qualified Health Centers (FQHCs), safety-net public health systems, or free clinics. These organizations are often underfunded, limiting their ability to provide testing, management, and followup services to their patients.
Lack of access to preventive medicine leads to increased risk of underlying health conditions such as obesity, hypertension, and diabetes—comorbidities that have been linked to more severe COVID-19 manifestations. In a national evaluation of health conditions in immigrant populations, 27.7% of those from Mexico, the Caribbean, and Central America had hypertension; 71.5% had obesity; and 9.6% had diabetes; compared with the age-adjusted prevalence of 45.4%, 42.4%, and 8.2%, respectively, in the U.S. general population. Within this population, the comorbidities tend to be higher in minority groups when compared to whites; for instance, while the prevalence of diabetes in the U.S. general population was 8.2% overall, it was 12.5% for people of Hispanic origin, 11.7% for non-Hispanic Blacks, and 7.5% for non-Hispanic whites.
Depending on their mode of entry into the United States, immigrants may also be at risk for excessive stress related to poverty, trauma, and poor social support, which leads to mental health conditions such as post traumatic stress disorder (PTSD), depression, and anxiety. These psychological stressors may be worsened during a pandemic, certainly for those with limited healthcare resources, high risk of job loss, or high risk of SARS-CoV-2 exposure.
Many immigrants are at increased risk both because their economic situation requires continuation of work despite social distancing and stay-at-home recommendations and because the types of jobs most commonly worked by immigrants often require face-to-face interactions. In Texas, immigrants make up more than 20% of the work force and are employed most commonly in the construction, hospitality, food services, healthcare, and manufacturing industries; these are “essential” professions that do not lend themselves to working from home. In addition, immigrants who continue working are more likely to use mass transit to get to their jobs, which further increases their risk of SARS-CoV-2 exposure.
In the home, immigrants are more likely to live in large, multigenerational family groups or with multiple roommates. Nearly 29% of Asian, 27% of Hispanic, and 26% of Black Americans live in multigenerational households, a practice that is particularly common in those who are foreign-born. If one person living in a crowded home is infected with SARS-CoV-2, their cohabitants, including elders and the immunosuppressed, will likely be exposed. In addition, recent immigrants and their families are less likely to have cell phones or internet access and to speak and read English. In Texas, for example, approximately 50% of undocumented immigrants lack English proficiency; consequently, they may be less likely to receive and understand public health messages, warnings, and updates.
Minority Children and COVID-19
[Material in this section is from Kim et al, 2020 unless otherwise cited.]
A recent CDC report reveals that minority children are disproportionately affected by COVID-19. Analysis of pediatric hospitalization data from 14 states from March 1 to July 25, 2020 found that although the cumulative rate of COVID-19–associated hospitalization among children (8.0 per 100,000 population) is low compared with that in adults (164.5), 1 in 3 hospitalized children was admitted to an intensive care unit (about the same rate as adults).
Most reported cases of COVID-19 in children under 18 years of age appear to be asymptomatic or mild. Less is known about severe COVID-19 illnesses requiring hospitalization of children. From March 21to July 25, weekly hospitalization rates steadily increased among children (from 0.1 to 0.4 per 100,000, with a weekly high of 0.7 per 100,000). Overall, Hispanic and Black children had higher cumulative rates of COVID-19–associated hospitalizations (16.4 and 10.5 per 100,000, respectively) than did non-Hispanic white children (2.1). Among 208 (36.1%) hospitalized children with complete medical chart reviews, 69 (33.2%) were admitted to an intensive care unit; 12 of 207 (5.8%) required invasive mechanical ventilation, and one patient died during hospitalization.
From March 1 to July 25, 576 children hospitalized with COVID-19 were reported to COVID-NET, a surveillance system that collects data on laboratory-confirmed COVID-19–associated hospitalizations in 14 states. Infants aged <3 months accounted for 18.8% of all children hospitalized with COVID-19. Among 526 children for whom race and ethnicity information were reported, 241 (45.8%) were Hispanic, 156 (29.7%) were Black, 74 (14.1%) were white; 24 (4.6%) were non-Hispanic Asian or Pacific Islander; and 4 (0.8%) were non-Hispanic American Indian/Alaska Native.
Overall weekly hospitalization rates among children increased steadily during the surveillance period (from 0.1 to 0.4 per 100,000, with a weekly high of 0.7 per 100,000). COVID-19–associated hospitalization rates were higher among Hispanic and Black children than among white children. The rates among Hispanic and Black children were nearly 8 times and 5 times, respectively, the rate in white children.
Although reasons for disparities in COVID-19-associated hospitalization rates by race and ethnicity are not fully understood, the highest rates of COVID-19–associated hospitalization were found among Hispanic children. Other recent studies have found a higher prevalence of COVID-19 infection in the Hispanic community as a whole, when compared to other racial and ethnic communities. It has been suggested that Hispanic adults are at increased risk for infection because they are overrepresented in essential and direct-service occupations with decreased opportunities for social distancing, which might also affect children living in those households.
Forty-two percent of children in the CDC analysis had one or more underlying medical conditions, with higher occurrences among Hispanic and Black children (45.7% and 29.8%, respectively) compared with white children (14.9%). This suggests that the greater prevalence of underlying conditions in minority children puts them at a higher risk for COVID-19-associated hospitalizations compared with white children.
This study and other studies of hospitalized children with COVID-19, found that obesity was the most prevalent underlying medical condition. Childhood obesity affects almost 1 in 5 U.S. children and is more prevalent in Black and Hispanic children. Recent studies have shown that even mild obesity is a major risk factor for hospitalization and critical illness (Gander, 2020).
Higher rates of multisystem inflammatory syndrome (MIS-C) are seen in children; this is a rare but serious complication of coronavirus that can lead to organ failure, shock, and death. More than 74% of the 570 of MIS-C cases reported to the CDC by July 29 were in Black and Hispanic children (Mascarenhas et al., 2020).
COVID-19 has severely impacted the American and global community, placing marginalized populations at high risk of contracting the virus and of developing severe COVID-19.
